About prostate cancer and HRR mutations
- Prostate cancer is:
- Prostate cancer can be grouped based on where the cancer has spread3:
- Localized prostate cancer is only in the prostate
- Locally advanced prostate cancer has spread outside the prostate but not to distant parts of the body, such as the lymph nodes
- Metastatic prostate cancer has spread beyond the prostate to distant parts of the body
Several clinical studies have indicated that 10% to 50% of prostate cancer cases progress to metastatic castration-resistant prostate cancer (mCRPC) within 3 years4
HRR mutations are more prevalent than you think
HRR mutations include BRCA1 and BRCA2 as the most common HRR gene mutations
Genetic aberrations, including those involving BRCA1/2, are significantly higher (19.3%) in patients with metastatic prostate cancer compared with those with advanced localized prostate cancer (5%)4
BRCA2 is the first (12% to 18%) most common altered gene involved in HRR1
BRCA1 is the fourth (<2%) most common altered gene involved in HRR1

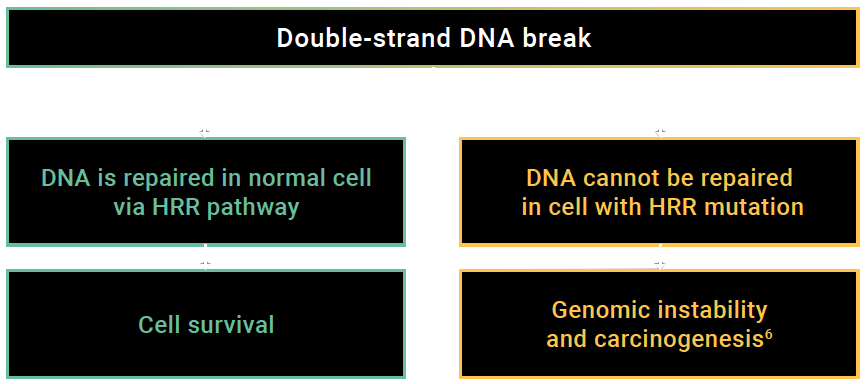
Homologous recombination repair gene mutations (HRR+) are a change in the nucleotide sequence of a gene involved in homologous recombination-type DNA 20 repair processes5
In a prospective cohort study, the presence of germline BRCA2 mutations reduced cause-specific survival by nearly half vs non-carriers (17.4 vs 33.2 months, 95% CI 1.07–4.10, p=0.27)1
Patients with HRR mutations have a genetically distinct disease driven by several mechanisms1:
Patients with deleterious HRR mutations in a cancer cell (called HRR+) have a genetically distinct disease that is driven by more than just androgen receptor (AR) signalling1
HRR positivity impairs prostate cancer cells’ ability to repair double-stranded DNA breaks via the normal HRR system1
DNA-damage response gene alteration induces a dependency on poly(adenosine diphosphate-ribose) polymerase (PARP), which binds to damaged DNA gaps1
Adapted from Scott R J, et al. 2021.4
Two key oncogenic pathways (somatic and germline) may contribute to tumour progression in prostate cancer: defective HRR and the androgen signalling axis. AR signalling regulates a network of DNA repair genes7
Somatic HRR gene alterations have been reported in8:
4.9%–22% of all prostate cancer patients
10%–16.4% of metastatic prostate cancer patients
Germline HRR gene alterations have been reported in9:
17.2%–19% of all prostate cancer patients
11.4%–11.8% of metastatic prostate cancer patients
7.5%–9.1% of metastatic castration-resistant prostate cancer patients
Somatic and germline mutations can be detected with multiple types of testing
| Methods | Sample Type |
|---|---|
Somatic testing4
| Tumour/metastatic tissue |
| Blood or saliva |
Circulating tumour DNA testing4
| Plasma |
*
Mutations in HRR genes commonly investigated in mCRPC include BRCA1, BRCA2, ATM, ATR, BARD1, BRIP1, CHK1/2, DSS1, CHEK2, CDK12, FANCA, NBN, PALB2, HDAC2, RAD51, RAD51B, RAD51C, RAD51D, RAD54L, and RPA1.4
BRCA1: Breast cancer gene 1
BRCA2: Breast cancer gene 2
HRR: Homologous recombination repair
mCRPC: Metastatic castration-resistant prostate cancer
PARP: Poly ADP-ribose polymerase
REFERENCES: 1. Teyssonneau D, Margot H, Cabart M, et al. J Hematol Oncol 2021;14(51):1–19.↵ 2. Brenner D, Poirier A, Woods R, et al. CMAJ 2022;194(7):E601–607.↵ 3. Canadian Cancer Society. 2021. Available: https://cancer.ca/en/cancer-information/cancer-types/prostate/staging.↵ 4. Scott RJ, Mehta A, Macedo GS, et al. Oncotarget 2021;12(16):1600–1614.↵ 5. National Cancer Institute Thesaurus. Available: https://ncit.nci.nih.gov/ncitbrowser/ConceptReport.jsp?dictionary=NCI_Thesaurus&version=22.11d&ns=ncit&code=C133695&key=1827865363&b=1&n=null.↵ 6. Minchom A, Aversa C, and Lopez J. Ther Adv Med Oncol 2018;10:1–18.↵ 7. Polkinghorn WR, Parker JS, Lee MX, et al. Cancer Discovery 2013;3(11):1245–1253.↵ 8. Lang S, Swift S, White H, et al. International Journal of Oncology 2019;55(3):597–616.↵ 9. National Cancer Institute Thesaurus. Available: https://ncit.nci.nih.gov/ncitbrowser/pages/concept_details.jsf;jsessionid=F3512613504D1CDED992BA49CAB9C463.↵